Multi-billion dollar chains of psychiatric facilities riddled with reports of abuse, accusations, and legal trouble. Recently, a psychiatric hospital in Dallas, TX announced it is closing its doors due to a report of another sexual assault on a patient under their care (CCHR International, 2018). A large number of psychiatric facilities have closed due to similar allegations. The closing of this particular facility will make it the 6th psychiatric hospital closing under its corporation. So, how does something so tragic happen over and over? Let’s dig deeper.
Tampa Bay Times published an award-winning series of articles investigating the state of Florida’s mental healthcare system beginning in 2009 and published in 2015. At that period of time, Florida cut $100 million from state-run mental hospitals. This budget cut resulted in firing over one-third of their workforce, the death of patients, injuries of staff members, and multiple lawsuits (Anton, Braga, & Cormier, 2015).
It is reported that over 55 people died in Florida state psychiatric hospitals in the years following this budget cut. The accurate numbers are difficult to uncover regarding the death of patients due to a number of reasons. Hospitals were able to withhold information regarding death of patients under a Florida Department of Children and Families (DCF) law if employees were not related to the death; however, this shroud of secrecy continued as state officials refused to report names of hospital employees associated with accidents by citing Florida law 415.107; which protects victims, those who report abuse, and the abusers.
Mortality reviews are required for hospital employees whenever a patient dies. If nothing is considered worth reporting, the investigation is sealed and not sent to DCF. A report by DCF is the only one who can publicly make investigation files visible. Family members of patients who died in state-run Florida psychiatric hospitals often were unable to know what happened to their loved ones. Security videos released to the public can be found on Tampa Bay Times’ website showing assaults made on patients, staff members, and among patients left unsupervised for long periods of time.
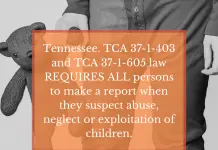
The examples available for highlighting failures of mental health facilities in the U.S. would take multiple volumes of books to cover. Tennessee has had its own troubles regarding mental healthcare facilities and policy. In recent years, a hospital in TN received harsh criticism after numerous documents were found in a dumpster owned by the facility containing patient information. As stated before, many of these horrific stories and failures are withheld from the public or take many years to make headlines; making it increasingly difficult to fully know the extent of allegations currently being processed. So, for this reason, we will be looking at these as relevant sources of information to allow us to understand why these failures occurred and perhaps what preventative measures could be taken.
It is not uncommon to hear mental health budgets being cut or reduced. As of 2017, data retrieved from World Atlas (2017) ranks Tennessee at 35th in terms of money allocated for mental health. One of TAT’s (Tennessee Advocacy Talk) previous articles highlights the struggles faced by those with mental illness in the Appalachian region of the U.S. Data from Mental Health America (2017) displays a map regarding access to care; the Southeastern U.S. ranks worse than any other region in the U.S. in multiple categories and mental health budget allocation.
With statistics like these available to us, it can be alarming to reflect on what has occurred in Florida and what could occur in other Southeastern states as a result of poor funding. The trickle-down effects of poor funding for mental healthcare do not only affect those seeking care, but it also puts a strain on those working in the mental health field. Facilities are often unable to pay reasonable wages that match the level of stress taken on by employees; especially those who are not in salaried positions. Even then, those with substantial amounts of education may choose to leave a facility for better-paying positions; leaving positions unfilled and just as Florida state-run hospitals laid off a third of their workforce as a result of budget cuts, patient numbers may remain steady despite state and federal guidelines. Situations like this create the ample opportunity for accidental death and injury to occur.
Other than lack of funding, which directly affects those with mental illness or those working in the mental health field, the existence of legal loopholes creates a large systemic problem regarding the report of accidents, abuse, and death. Just as families of patients in Florida’s state psychiatric hospitals were left confused and desperate, state laws can create legal loopholes for facilities that allow them the ability to withhold information regarding death, injury, and abuse of patients depending on the context of the precipitating events. This does not include the possibility of modifying documentation to minimize a facility’s responsibility.
If you find this article particularly interesting or alarming, feel free to drop us a comment or message. We love to hear from our readers in response to the current status of mental health care in TN and nationally. Keeping these statistics in mind, let others know that mental health still has a long way to go in order to match more progressive states. Stay tuned for future articles and news.
References
Psychiatric Hospital Rife With Sexual Assault Allegations Finally Shuts Down While Another Faces Lawsuit over Teen Rape
http://www.tampabay.com/projects/2015/investigations/florida-mental-health-hospitals/secrecy/
https://www.tennessean.com/story/money/industries/health-care/2015/03/19/state-probes-mental-health-facilitys-trashed-paperwork/25051043/
https://www.worldatlas.com/articles/states-who-spend-the-most-on-mental-health-funding.html
http://www.mentalhealthamerica.net/issues/mental-health-america-access-care-data